
Endometriosis is a condition in which cells of the lining of the uterus, which usually fall with the menstrual bleeding, implant and grow in areas outside the womb, such as the pelvis, ovaries, and more. Symptoms include severe menstrual cramps, pain during intercourse, increased menstrual bleeding, infertility, and more.
Chronic pelvic pain is a pain that is not only during menstruation, but also lasts for over 6 months (continuous or alternating), and it interferes with the quality of life or normal functioning. The source of the pain may be gynaecological, digestive, urinary, skeletal, or neurological. The common cause of chronic pelvic pain is endometriosis.
Suffering from menstrual cramps? Pain during intercourse?
Endometriosis is the leading cause of menstrual pain, chronic pelvic pain, sub-fertility, and other symptoms. Most GP’s, think that menstrual pain is a normal phenomenon, so the diagnosis of endometriosis is delayed. The average time in the world, from the time the woman first visits the doctor until diagnosis, is 8 years! Many women suffer from such intense pain that they are confined to bed and painkillers, missing school, work, physical or social activity around the period. This is a serious interference to the quality of life, and this is an abnormal situation. In other cases, women who suffer from severe pain during intercourse, avoid sexual contact, which is also abnormal.
Today, awareness of endometriosis is increasing worldwide, due to the high percentage of women suffering from the phenomenon and the treatment options that have developed.
What is endometriosis?
Endometriosis is a condition in which endometrial cells, which fall out/shed every month with the menstrual cycle, implant and grow in areas outside the womb. The most common area is the pelvis and around the ovaries, but may be located anywhere in the body, even in the lung and brain.
Endometriosis causes pain in several ways:
- Endometriosis tissue bleeds every month in the same way as in the womb, but in a foreign location, the bleeding will cause pain.
- The cells that are implanted in foreign tissue create changes around them such as fibrosis and pressure on local nerves.
- Endometriosis cells secrete inflammatory substances that cause pain.
- Endometriosis creates adhesions between organs in the pelvis where it grows. Adhesions cause pain.
Prevalence of Endometriosis
It is estimated that about 5%-10% of all women of childbearing age will suffer from symptoms associated with endometriosis.
Up to 45% of all women with infertility will be diagnosed with endometriosis during infertility investigation. About 40% of all women with chronic pelvic pain will be diagnosed with endometriosis.
Symptoms
The symptoms of endometriosis vary widely from woman to woman and the severity of symptoms is not necessarily related to the severity of the disease. Symptoms depend on the extent and location of the endometrial implants and the affected structures. While some women have few or no symptoms, others experience severe and incapacitating pain that recurs each month for many years.
- Period pain
- Pain during sexual intercourse
- Pelvic and abdominal pain outside of menstruation
- Abnormal bleeding – heavy/prolonged/irregular bleeding, clotting
- Difficulty in getting pregnant
- Painful urination and bowel disturbance
- Premenstrual syndrome
The anticipation of recurrent pain each month can lead to a feeling of anxiety, stress and depression.
Other causes of chronic pelvic pain
Gynaecological causes: adhesions following surgery or infection, ovarian cysts, venous congestion syndrome.
Gastrointestinal tract: inflammatory bowel disease (Crohn’s disease, ulcerative colitis), diverticulitis
Urinary tract: Interstitial cystitis, chronic infection
Neural: Pressure one of the pelvic nerves.
How is Endometriosis diagnosed?
The gold standard diagnosis is by imaging the lesions in laparoscopy or histologicall verification of the lesions that have been removed during laparoscopy. Nevertheless, one can almost certainly say that a woman has endometriosis, according to the characteristic symptoms, history, and a good response to hormonal therapy.
Physical examination and pelvic ultrasound can support but not exclude the diagnosis, as in many patients there will be no findings on both.
Treatment
Treatment for endometriosis depends on a number of factors including:
- The severity of symptoms
- The extent of the endometriosis
- The woman’s age
- Her outcome requirements and goals (e.g. reduction in pain, improved lifestyle and improved fertility).
No treatment can absolutely prevent endometriosis from recurring but a combination of regular medical follow-up, hormonal treatment and/ or surgery, can control the disease.
Medical treatment
Drug therapy is essential for the suppression of endometriosis and its effects. Treatment includes hormonal effect and suppression of inflammatory factors that are secreted from the lesions. Just as hormones affect the menstrual cycle, it will affect endometriosis tissue and inhibit its growth. For maximum results, hormonal suppression should be used regularly, except when trying to conceive.
Medications used include:
- The oral contraceptive pill, Implanon
- Anti-inflammatory medications
- Mirena IUD
- Hormonal suppression treatment – Zoladex
Anti-inflammatory drugs belonging to the NSAIDS family include Ibuprofen, Ponstan, Voltaren, etc.
Surgical treatment
Surgery is recommended in the following situations:
- For the purpose of diagnosing and treating a disease that causes severe symptoms that impairs the functioning and quality of the woman’s life.
- When there is no adequate response to drug therapy.
- When there are significant findings in sonar examination – anatomical distortion, bladder or intestinal infiltration, large cysts.
- Emergency conditions associated with endometriosis – rupture or torsion of cyst, bowel obstruction, etc.
- Investigation and treatment of infertility.
Aims of the surgical treatment:
- Reduce pain and relieve symptoms
- Restoring proper anatomy
- Removing lesions
- Separation of adhesions
- Confirm patency of the fallopian tubes
How is the surgical treatment done?
- Today, most operations are done in a laparoscopic approach. In laparoscopy, the patient earns small scars and relatively quick recovery. For the surgeon, the laparoscopic device enables closer examination of the findings, identification of small lesions, and performing finer surgical procedures. In the procedure, the adhesions are separated and as many lesions as possible are removed, without damage to vital organs and in an attempt to preserve the ovaries and the uterus. The surgery reduces pain and can improve fertility.
- A hysterectomy is reserved for women who have completed family planning and whose hysterectomy is thought to improve the quality of their lives. A hysterectomy helps improve symptoms, usually for women with adenomyosis (a type of endometriosis, in which the endometriosis cells implant inside the uterine wall).
Personal consultation, examination and coordination of expectations are very important before deciding on surgery.
Alternative medicine can assist with reducing pain, and is worth trying:
- Acupuncture
- Ervigo- uterine massage
- Anti inflammatory diet
Any treatment needs to be individualized to each patient bearing in mind the severity of symptoms, extent of endometriosis, and the overall goals of treatment.
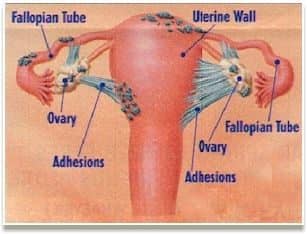
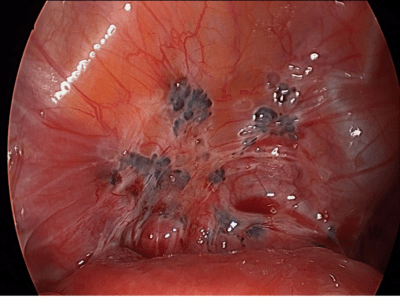
Samples of Endometriosis
Different locations of endometriosis lesions on the uterus, ovaries and fallopian tubes
g
Endometriosis on the bladder surface (black, white lesions and adhesions)
GG
FAQs
What is chronic pelvic pain syndrome?
Chronic pelvic pain is a pain in the area below your belly button and between your hips that lasts six months or longer. The pain can be constant or come and go but remains in the same area. Menstruation, ovulation, intercourse, bowel motion, voiding and physical activity can aggravate the pain. Pelvic pain can also be associated with other symptoms such as feeling ill, nauseated, bloated and more.
Chronic pelvic pain develops over several years and usually increases and extends longer with time.
Can chronic pelvic pain be cured or go away?
Depending on the cause of the pain, some causes can be treated with good results and some are more difficult to resolve but the pain can be eased.
What causes chronic pelvic pain?
There are multiple causes for chronic pelvic pain. It can be a symptom of another disease, or it can be a condition in its own right. The most common cause is Endometriosis or Adenomyosis but could be: pelvic adhesions, irritable bowel syndrome, pelvic vein congestion, interstitial cystitis, chronic pelvic inflammatory disease, fibroids, pelvic floor muscle spasm, vulvodynia and psychological issues.

